Let me share something that genuinely frustrates me after two decades managing ENT protocols: people assume all stuffy noses are identical, when reality involves at least six distinct causes requiring completely different treatment approaches for optimal results.
The blocked nose from spring allergies operates through entirely different mechanisms than viral cold congestion, which differs again from bacterial sinusitis, irritant exposure, structural abnormalities, or medication side effects.
Throwing random decongestants at every type of congestion wastes money whilst delaying appropriate treatment—understanding your specific cause determines which interventions actually work versus which prove useless or counterproductive.
Allergic Congestion Mechanisms
Histamine release from mast cells drives allergic nasal congestion—immune overreaction to harmless substances triggering inflammatory cascade swelling nasal tissues within minutes of exposure.
Antihistamines block histamine receptors preventing inflammatory signals—first-line treatment for allergic congestion whilst largely ineffective for non-allergic causes lacking histamine involvement.
Nasal corticosteroids reduce allergic inflammation at source—superior long-term control compared to antihistamines for chronic exposure situations like seasonal allergies or pet dander.
The distinguishing features include clear watery discharge, sneezing, itchy nose and eyes—symptom constellation pointing toward allergic rather than infectious or irritant causes.
Environmental control through allergen avoidance dramatically reduces treatment requirements—identifying and eliminating triggers works better than endless medication managing preventable exposures.
What clinical experience demonstrates is that allergic congestion responds poorly to simple decongestants—treating inflammation proves more effective than just temporarily shrinking swollen tissues without addressing underlying cause.
Viral Infection Patterns
Rhinoviruses and other cold viruses directly damage nasal epithelium triggering inflammatory repair response—congestion results from combination of viral damage and body’s defensive reaction.
Decongestants provide symptomatic relief but don’t address viral infection—reduce swelling temporarily whilst immune system fights actual cause over 7-10 day natural course.
Anti-inflammatory treatments reduce excessive immune response—moderate inflammation assists healing, but overactive response creates more suffering than necessary for viral clearance.
The characteristic progression involves initial clear discharge becoming thicker and discolored as immune cells accumulate—normal progression not indicating bacterial infection requiring antibiotics.
Supportive care through hydration, rest, and symptom management works better than aggressive pharmaceutical intervention—body resolves viral infections naturally when properly supported.
The critical distinction from allergies involves absence of itching, presence of systemic symptoms like fatigue and body aches, and self-limiting course improving after initial worsening.
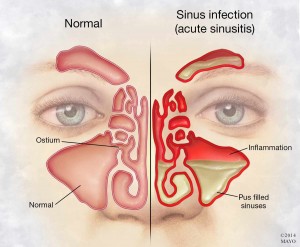
Bacterial Sinusitis Development
Bacterial superinfection develops when viral inflammation blocks sinus drainage—stagnant mucus becomes infected requiring antibiotic treatment simple decongestants can’t provide.
Extended duration beyond 10 days or improvement followed by worsening suggests bacterial involvement—viral infections don’t last weeks or show biphasic patterns indicating secondary infection.
Antibiotics target bacteria whilst decongestants and irrigation restore drainage—combination approach addresses infection and promotes clearance preventing recurrence after antibiotic completion.
The diagnostic features include facial pain, pressure over sinuses, thick discolored discharge, and fever—constellation suggesting bacterial involvement rather than simple viral or allergic congestion.
Imaging and cultures confirm bacterial sinusitis but aren’t routinely necessary—clinical diagnosis based on symptoms guides treatment in most cases reserving advanced testing for complicated or recurrent situations.
What separates bacterial from viral congestion is treatment urgency—viral infections resolve naturally whilst bacterial sinusitis requires antibiotics preventing complications like orbital cellulitis or intracranial spread.
Irritant and Environmental Causes
Chemical irritants, smoke, pollution, and dry air trigger non-allergic non-infectious inflammation—nasal tissues react defensively to noxious exposures without immune or infectious involvement.
Removal from irritant environment plus nasal irrigation clears reactive congestion—simple environmental modification proves more effective than medication treating symptoms without eliminating ongoing cause.
Vasomotor rhinitis involves exaggerated response to temperature changes, strong odors, or spicy foods—neural reflex rather than allergic or infectious process requiring different management approach.
The defining characteristic is direct temporal relationship between exposure and symptoms—immediate congestion upon contact with triggers that quickly improves after exposure cessation.
Medication provides limited benefit when ongoing exposure continues—treating symptoms while remaining in problematic environment creates frustrating cycle of temporary relief and prompt recurrence.
The fundamental solution involves environmental control—workplace modifications, air purification, smoking cessation, or humidity optimization addresses root cause making treatment largely unnecessary.
Structural and Chronic Issues
Deviated septum, nasal polyps, or turbinate hypertrophy create mechanical obstruction—physical blockage rather than inflammation meaning medical treatments provide limited improvement.
Surgical correction may become necessary for structural problems—medications manage symptoms temporarily but can’t fix anatomical issues causing persistent obstruction despite aggressive treatment.
Chronic rhinosinusitis involves persistent inflammation from various causes—requires sustained treatment and sometimes prolonged antibiotics or surgical intervention beyond simple acute congestion management.
The distinguishing feature is persistence despite appropriate treatment—congestion lasting months rather than days or weeks suggests structural or chronic inflammatory problems requiring specialized evaluation.
Medication side effects from blood pressure drugs, antidepressants, or overused nasal sprays cause congestion—requires medication adjustment rather than adding more treatments worsening the problem.
What extensive clinical experience teaches is that some congestion requires addressing underlying systemic issues—treating the symptom alone proves futile when root cause continues operating.
Tailoring Treatment to Specific Causes
Effective congestion management requires accurate cause identification—allergic congestion needs antihistamines whilst bacterial infection requires antibiotics and viral congestion responds to supportive care.
One-size-fits-all approaches fail consistently—shotgun treatment wastes resources while proper diagnosis directs therapy efficiently toward actual problem mechanisms.
What two decades of practice has demonstrated repeatedly is that understanding why you’re congested determines treatment success—mechanism-directed therapy outperforms generic approaches dramatically.
FAQs
How do I know if congestion is allergic or infectious?
Allergies involve itching, clear discharge, and exposure relationship. Infections include systemic symptoms, yellow/green discharge, and temporal progression. Timing and associated symptoms usually distinguish them clearly.
When does viral congestion become bacterial?
After 10+ days, with worsening after initial improvement, severe symptoms including high fever and facial pain. Most colds don’t become bacterial—this progression occurs in minority requiring medical evaluation.
Can I have multiple causes simultaneously?
Yes. Allergic rhinitis plus viral infection, or dry air irritation plus medication side effects commonly co-exist. Treatment must address all contributing factors for complete resolution.
Why doesn’t my usual decongestant work anymore?
Cause likely differs from previous episodes. Decongestants work for vascular swelling but not structural blockage, certain infections, or specific inflammatory patterns. Reassess the underlying cause.
Should I see a doctor for every stuffy nose?
No. Most resolve naturally within a week. Seek evaluation for symptoms beyond 10 days, severe pain, high fever, vision changes, recurrent episodes, or lack of response to appropriate treatment.
Can weather cause congestion without allergens?
Yes. Temperature and humidity changes trigger vasomotor rhinitis—neural reflex causing congestion without allergic or infectious involvement. Common in cold weather or air-conditioned environments.
Why is one nostril always more blocked?
Normal nasal cycle alternates dominant airflow between nostrils every few hours. Congestion exaggerates this natural pattern. Persistent one-sided blockage may indicate structural problems requiring evaluation.
Do I need antibiotics if discharge turns yellow?
Not necessarily. Color change reflects immune cell accumulation normal in viral infections. Duration, severity, and other symptoms determine bacterial involvement—color alone doesn’t indicate antibiotic need.
Can stress cause nasal congestion?
Indirectly. Stress affects immune function and inflammatory responses potentially worsening existing congestion or increasing susceptibility to triggers. However, stress alone doesn’t directly cause congestion.
Why does congestion persist after treating the cause?
Inflammation takes time resolving after trigger removal. Damaged tissues require healing even after infection clears or allergen exposure stops. Continued symptoms 2-3 weeks post-treatment warrant re-evaluation.